Aku dan Lensa Hidup
Hanya pendapat,ilmu dan pengalaman....
Saturday, 18 April 2020
Thursday, 30 January 2020
Saturday, 29 September 2018
Common Medical Devices (Oxygen Delivery Devices)
Today I want to share about common medical devices used in emergency/ hospital and clinic setup. For medical students, you all may use this as your revision for your OSCE.
A) Oxygen Delivery Devices
1. Nasal Cannula

What?
-It is a disposable, plastic device with a two protruding prongs for insertion into nostrils, connected to an oxygen source.
Indication?
-used to deliver low flow oxygen
-patient is stable
Contraindication
-nasal blockage
-facial injuries
Advantages
-easily used
-safe and simple
-easily tolerated
Disadvantages
-unable to use with nasal obstruction
-drying to mucous membrane
-can dislodge from noses easily
-causes skin irritation or breakdown over ears.
2. Simple face mask
What?
-simple mask is made of clean, flexible, plastic or rubber that can be molded to fit the face.
Indication
-medium flow oxygen
-respiratory acidosis
Contraindication
-poor respiratory effort
-severe hypoxia
-apnea
Advantages
-can provide increased delivery of oxygen for short period of time.
Disadvantages
-tight seal required to deliver higher concentration
-difficult to keep mask in position over nose and mouth
-uncomfortable for patient while eating or talking.
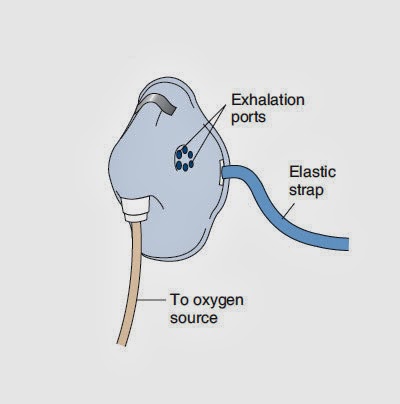
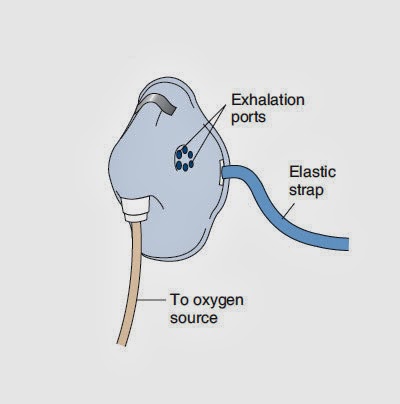
3. Non-rebreathing face mask

Character
-two one-way valve
Indication
-delivery of high concentration of oxygen
-chronic airway limitation
Contraindication
-poor respiratory effort
-apnea
Advantages
-delivers the highest possible oxygen concentration
-suitable for patient breathing spontaneous with severe hypoxemia.
Disadvantages
-impractical for long term therapy
-expensive
-feeling of suffocation
-uncomfortable
4. Venturi mask
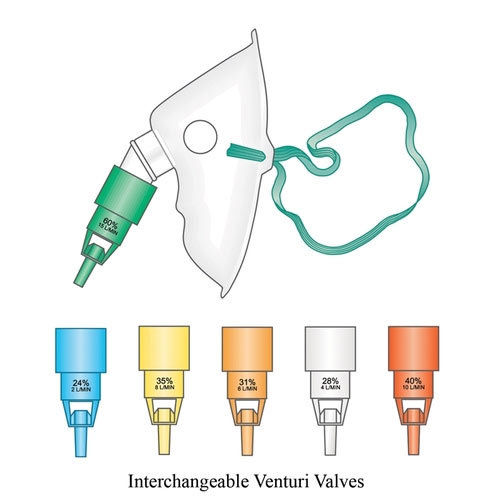
What?
-disposable face mask used to deliver a controlled oxygen concentration to patient.
-high flow oxygen mask.
-designed to allow inspired air to mix with oxygen.
Indication
-COPD
-Acute respiratory disease
Contraindication
-Poor respiratory efforts
-apnea
-severe hypoxia
Special precaution
-monitor SaO2 with pulse oximeter
-make sure the valve connected and function properly
-have risk of skin irritation.
5. Nebulizer mask

What?
-Is a drug delivery device used to administer medication in the form of a msit that is inhaled into the lungs.
Indication
-Administration of bronchodilators (salbutamol) in asthma and COPD
-Administration of corticosteroids such as (budesonide) in asthma patient
-Administration of mucolytic and antimicrobial in bronchiectasis and cystic fibrosis
-hypertonic saline to improve mucociliary clearance and lung function in patients with cystic fibrosis.
6. BVM Ventilator

Indication
-failure of ventilation or oxygenation
-failed intubation
Contraindication
-complete upper airway obstruction
-after induction
-after paralysis
Complication
-aspiration
-hypoventilation
7. Pulse oximeter

What?
-Is a non invasive method allowing the monitoring of oxygenation of patients hemoglobin.
Indication
-to monitor oxygen saturation in diseased states
-to monitor responsiveness to therapy
-to monitor side effect during procedures
-to detect blood flow in endagered body regions
Normal reading
-95% - 99%
Approach (technique)
-digit
-ears
-forehead
-palm / foot in neonates
A) Oxygen Delivery Devices
1. Nasal Cannula

What?
-It is a disposable, plastic device with a two protruding prongs for insertion into nostrils, connected to an oxygen source.
Indication?
-used to deliver low flow oxygen
-patient is stable
Contraindication
-nasal blockage
-facial injuries
Advantages
-easily used
-safe and simple
-easily tolerated
Disadvantages
-unable to use with nasal obstruction
-drying to mucous membrane
-can dislodge from noses easily
-causes skin irritation or breakdown over ears.
2. Simple face mask
What?
-simple mask is made of clean, flexible, plastic or rubber that can be molded to fit the face.
Indication
-medium flow oxygen
-respiratory acidosis
Contraindication
-poor respiratory effort
-severe hypoxia
-apnea
Advantages
-can provide increased delivery of oxygen for short period of time.
Disadvantages
-tight seal required to deliver higher concentration
-difficult to keep mask in position over nose and mouth
-uncomfortable for patient while eating or talking.
3. Non-rebreathing face mask
Character
-two one-way valve
Indication
-delivery of high concentration of oxygen
-chronic airway limitation
Contraindication
-poor respiratory effort
-apnea
Advantages
-delivers the highest possible oxygen concentration
-suitable for patient breathing spontaneous with severe hypoxemia.
Disadvantages
-impractical for long term therapy
-expensive
-feeling of suffocation
-uncomfortable
4. Venturi mask
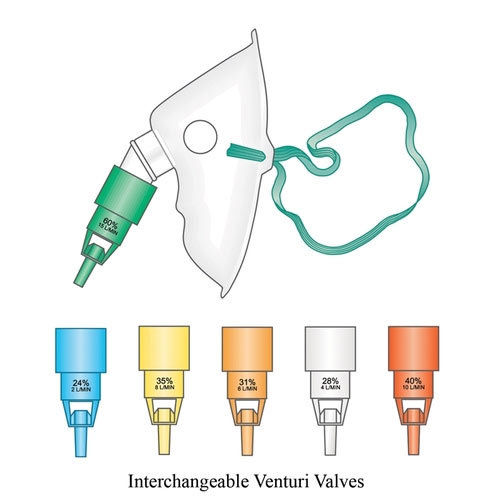
What?
-disposable face mask used to deliver a controlled oxygen concentration to patient.
-high flow oxygen mask.
-designed to allow inspired air to mix with oxygen.
Indication
-COPD
-Acute respiratory disease
Contraindication
-Poor respiratory efforts
-apnea
-severe hypoxia
Special precaution
-monitor SaO2 with pulse oximeter
-make sure the valve connected and function properly
-have risk of skin irritation.
5. Nebulizer mask

What?
-Is a drug delivery device used to administer medication in the form of a msit that is inhaled into the lungs.
Indication
-Administration of bronchodilators (salbutamol) in asthma and COPD
-Administration of corticosteroids such as (budesonide) in asthma patient
-Administration of mucolytic and antimicrobial in bronchiectasis and cystic fibrosis
-hypertonic saline to improve mucociliary clearance and lung function in patients with cystic fibrosis.
6. BVM Ventilator

Indication
-failure of ventilation or oxygenation
-failed intubation
Contraindication
-complete upper airway obstruction
-after induction
-after paralysis
Complication
-aspiration
-hypoventilation
7. Pulse oximeter

What?
-Is a non invasive method allowing the monitoring of oxygenation of patients hemoglobin.
Indication
-to monitor oxygen saturation in diseased states
-to monitor responsiveness to therapy
-to monitor side effect during procedures
-to detect blood flow in endagered body regions
Normal reading
-95% - 99%
Approach (technique)
-digit
-ears
-forehead
-palm / foot in neonates
Thursday, 27 September 2018
Tutorial Cara Download File Torrent Jadi Direct Link
Biasa kalau internet yang tak boleh nak P2P, akan ada masalah bila nak download file torrent. So, hari ni aku nak ajar korang macam mana nak download file torrent jadi direct link download. Mula-mula, korang download dulu file torrent.
Kalau movie aku suka download kat https://yts.am/
Then, korang cari la movie yang korang nak download. Macam contoh, aku nak download cite Solo Star Wars tu. Then, aku tekan la gambar poster movie Solo tu.
Jadi, dia akan keluar benda camni. Then, korang tekan download yang warna hijau bawah poster movie tu.
Kemudian, korang pilih la kualiti yang mana korang nak. Lagi tinggi kualiti, lagi besar file download dan lagi lama masa menunggu. Aku pilih yang kualiti 720p je sebab yang tu pun dah lawa.
Bila korang dah download, korang akan dapat file ni. Ni la file torrent tu.
Kemudian, korang bukak website ni https://www.seedr.cc
Korang kena daftar dulu tau. Alaa free jer pun.Tekan sign up tu.
Nanti dia keluar macam gambar kat atas ni. Then, file torrent yang korang download tadi, korang drag je masuk sini.
Bila dah masukkan file tadi, korang gerakkan cursor mouse korang ke file tadi. Nanti ada 3 benda yang dia akan muncul. Yang aku bulatkan dalam pen merah tu, tu butang download. Korang boleh tekan je kalau tak menyabo. Tapi macam aku, browser aku slow kalau nak download file besar2. Kadang2, dia putus sendiri. So, penyelesaian aku, korang right click yang simbol aku bulatkan merah tu.
Nanti akan keluar benda ni. Lepastu korang tekan 'Copy Download Link'. Lepas korang dah tekan, korang bukak apps 'Internet Download Manager'.
Kemudian, korang tekan 'Add URL' yang kat atas belah kiri sekali yang warna kuning tu.
Then, dia akan keluar macam ni. So, korang paste je link yang korang copy tadi kat situ. Lepastu tekan OK.
Korang tunggu jap. Bila dia keluar gambar buku tu dengan berapa MB atau GB file korang, baru korang boleh tekan download. Then, Siap!
Oh lupa pulak, yang pasal website https://www.seedr.cc tu, korang ada limit 2GB je tau. Kalau nak lebih korang kena beli. Tapi korang jangan risau, bila dah habis download movie/file korang, korang bole drag balik file movie lain. Dun worry. Kalau movie korang kurang daripada 1gb, so korang boleh letak 2 file dalam satu masa. Bila dah habis download, buang la. Senang kan?
Share tips/tutorial ini kalau membantu :)
Kalau movie aku suka download kat https://yts.am/
Then, korang cari la movie yang korang nak download. Macam contoh, aku nak download cite Solo Star Wars tu. Then, aku tekan la gambar poster movie Solo tu.
Bila korang dah download, korang akan dapat file ni. Ni la file torrent tu.
Kemudian, korang bukak website ni https://www.seedr.cc
Korang kena daftar dulu tau. Alaa free jer pun.Tekan sign up tu.
Nanti dia keluar macam gambar kat atas ni. Then, file torrent yang korang download tadi, korang drag je masuk sini.
Bila dah masukkan file tadi, korang gerakkan cursor mouse korang ke file tadi. Nanti ada 3 benda yang dia akan muncul. Yang aku bulatkan dalam pen merah tu, tu butang download. Korang boleh tekan je kalau tak menyabo. Tapi macam aku, browser aku slow kalau nak download file besar2. Kadang2, dia putus sendiri. So, penyelesaian aku, korang right click yang simbol aku bulatkan merah tu.
Kemudian, korang tekan 'Add URL' yang kat atas belah kiri sekali yang warna kuning tu.
Then, dia akan keluar macam ni. So, korang paste je link yang korang copy tadi kat situ. Lepastu tekan OK.
Korang tunggu jap. Bila dia keluar gambar buku tu dengan berapa MB atau GB file korang, baru korang boleh tekan download. Then, Siap!
Oh lupa pulak, yang pasal website https://www.seedr.cc tu, korang ada limit 2GB je tau. Kalau nak lebih korang kena beli. Tapi korang jangan risau, bila dah habis download movie/file korang, korang bole drag balik file movie lain. Dun worry. Kalau movie korang kurang daripada 1gb, so korang boleh letak 2 file dalam satu masa. Bila dah habis download, buang la. Senang kan?
Share tips/tutorial ini kalau membantu :)
Wednesday, 26 September 2018
Senarai Case Write Up (CWU)
Ni aku nak kongsi dengan korang CWU yang aku buat masa jadi medical student. Ada yang aku clerk sendiri dan ada yang aku cari kat internet.
Internal Medicine
1. Pulmonary Tuberculosis
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-internal-medicine.html
Paediatric
1. UTI (Urinary Tract Infection)
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-pediatrik-urinary-tract.html
2. Pneumonia
https://nikmuhamadariff.blogspot.com/2018/09/cwu-pneumonia-paediatric.html
O&G
1. Ectopic Pregnancy
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-o-ectopic-pregnancy.html
2. Diabetes complicating pregnancy
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-o-diabetes-complicationg.html
3. Ovarian cyst
https://nikmuhamadariff.blogspot.com/2018/09/cwu-gynae-ovarian-cyst.html
Surgery
1. Stomach CA
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-surgery-stomach-ca.html
2. Breast Ca
https://nikmuhamadariff.blogspot.com/2018/09/case-wriye-up-surgery-breast-cancer.html
Harap membantu korang siapkan CWU. Nanti kalau ada lagi, aku update lagi.
Internal Medicine
1. Pulmonary Tuberculosis
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-internal-medicine.html
Paediatric
1. UTI (Urinary Tract Infection)
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-pediatrik-urinary-tract.html
2. Pneumonia
https://nikmuhamadariff.blogspot.com/2018/09/cwu-pneumonia-paediatric.html
O&G
1. Ectopic Pregnancy
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-o-ectopic-pregnancy.html
2. Diabetes complicating pregnancy
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-o-diabetes-complicationg.html
3. Ovarian cyst
https://nikmuhamadariff.blogspot.com/2018/09/cwu-gynae-ovarian-cyst.html
Surgery
1. Stomach CA
https://nikmuhamadariff.blogspot.com/2018/09/case-write-up-surgery-stomach-ca.html
2. Breast Ca
https://nikmuhamadariff.blogspot.com/2018/09/case-wriye-up-surgery-breast-cancer.html
Harap membantu korang siapkan CWU. Nanti kalau ada lagi, aku update lagi.
Case Write Up Internal Medicine (Pulmonary Tuberculosis)
Patient Details
Name : Zakaria bin
Abdullah
Age : 52 years old
Gender : Male
Race : Malay
Religion : Muslim
Address : Setapak,
Kuala Lumpur
Date of clerking :
22/01/2018
Date of admission
: 21/01/2018
Chief Complaint
Patient came to
the hospital due to chest pain past 1 months
History of Presenting Illness
Patient is not
known of any medical illness and never admitted to ward before. Prior to
admission the illness started with fever for 1 month. It started gradually at
night while the patient was resting and intermittent in nature. The fever was
high grade but patient denies of having chills, rigor or sweating. It was
associated with malaise and was not relieved by the use of Paracetamol.
Then, patient
started having chest pain suddenly about one hour after having the fever. The
pain was localized at the left axillary area. It was sharp in nature and
initially lasted for about 10 minutes. It occurred about twice a day at random
times with severity of 4 from 10. After about two weeks, it progressively worse
to a peak prior to admission with a frequency of at least 5 times a day,
lasting about 10 minutes each for each episode at random times of the day with
a severity of 8. There was no radiation of pain. The pain was relieved by the
use of illicit drugs such as morphine and there are no exacerbating factors. It
is associated with weight loss of 7kg (61 to 54kg) in the last two months.
There was no cough, dyspnea, hemoptysis, sputum production, leg swelling, decreased
exercise tolerance, night sweats, orthopnea and PND.
Past Medical History
The patient was
not a known case of any medical condition prior to this episode.
No previous
history of any hospitalization before this.
Past Surgical History
Patient has not
undergone any surgery before.
Past Medication History
The patient was
not on any known medication.
There was no
prescribed, over-the-counter and traditional medication used.
Allergy History
The patient is
allergic to seafood and suffers from red rashes all over the body upon
consumption. Otherwise the patient is not known to be allergic to any other
food or medication.
Family History
His father was
passed away at the age of 50 due to suicide with no known underlying medical
illness.
His mother was
divorced and left the family when he was still young.
His four siblings
aged 55, 54, 53 and lastly 50 respectively.
His elder brother
passed away at the age of 53 last year in 2016 due to complications related to
AIDS.
Otherwise, there
were no history of similar medical problems, malignancy or congenital defects
in the family.
Social History
Patient is a
chronic smoker started at the age of 17 with 3 packs of cigarettes a day.
He is an illicit
drug user which was methamphetamine, marijuana and currently on morphine.
He denies of any
use of intravenous drug use.
Otherwise the
patient claimed to not have consume alcohol, maintain a strict diet nor
exercise regularly.
There was poor
social support system with a poor relationship with the family members, all of
whom are also illicit drug users except his mother.
He is living on
the streets at Setapak near mosque.
He is currently
unemployed. A social welfare officer approached him two weeks ago, and since
then he has been staying in Renewal Life Home, which is a place that homes
rehabilitating drug addicts.
It was a crowded
place and always had contact with foreign workers. Among his friends whom is a
known case of tuberculosis for the past one year and currently not on any form
of treatment or follow-ups. He claimed to have had only a single partner
before. His last occasion was more than 10 years and claimed used to be
frequent. He also claimed uses no protection.
Review of Systems
CVS : No
palpitations, tachycardia, orthopnea or paraxosymal nocturnal dyspnea (PND)
GIT : No change in
appetite or bowel habits with no nausea, constipation, diarrhoea, melena,
vomiting or abdominal pain.
MSK : No muscle or
joint pain, redness or swelling of joints.
URI : No
frequency, urgency, hematuria or dysuria.
ENDOCRINE : No
temperature intolerance, excessive sweating or increased thirsty.
CNS : No headache,
fainting, tremors or fits.
Summary
Mr Z is a 52 years
old Malay male who presented with a chief complaint of fever and chest pain for
the past one month. The patient is a chronic smoker and illicit drug user for
the past 35 years. The patient has a poor socioeconomic background with history
of contact with a known tuberculosis patient.
General Examination
The patient is an
old age Malay male with an average height and is slightly cachexic. He is
alert, conscious and responsive and is not in any pain or distress. He is
oriented to time, place and person.
There is a branula
attached to his right hand and a chest tube attached to his left chest wall
along the axillary line.
Vital signs
|
CRITERIA
|
VALUES
|
|
Temperature
|
37.0
˚C
|
|
Blood
Pressure
|
138/88
mmHG
|
|
Pulse
Rate
|
100
beats per minute
|
|
Respiratory
Rate
|
20
breaths per minute
|
|
Body
Height
|
170
cm
|
|
Body
Weight
|
54
kg
|
|
BMI
|
18.7
kg/m2
|
Hands
The hands were
moist, pink and warm. There are no signs of pallor or peripheral cyanosis.
Capillary refill time is less than 2 seconds. There was no clubbing, tar
stains, fine tremors, palmar erythema, wasting of muscles, asterixis, Janeway
lesions, Osler nodes & splinter haemorrhage.
Face
There was no
facial edema, ptosis or miosis
Eyes
The patient’s eyes
show equally dilated pupils that is reactive to light.
There was no
corneal arcus, pallor or jaundice.
Nose
There was no
abnormal shape of the nose with no nasal discharge, nasal polyp or deviated
nasal septum.
Mouth
The oral hygiene
is poor. Otherwise the hydration status is good with no central cyanosis or
ulcers.
Neck
There was no
raised JVP, tracheal deviation or cervical lymphadenopathy.
Legs
There was no pedal
oedema on both legs and dorsalis pedis pulse was felt on both legs.
Respiratory Examination
Inspection
There is a pectus
excavatum deformity of the chest wall.
Otherwise it was
symmetrical and no scars seen.
Palpation
The apex beat was
palpable on the 5th intercostal space at the midclavicular line.
Chest expansion
was reduced on the left side.
Percussion
The percussion
noted was slightly dull on the left inframammary area but is otherwise resonant
in all other areas.
Tactile fremitus
is lightly reduced on the left inframammary region.
Auscultation
Air entry is
reduced on both sides.
There was
bronchial breath sounds heard with a short inspiratory and expiratory phase
with no other added lung sounds.
Cardiovascular Examination
Inspection
There is pectus
excavatum deformity of the chest wall but is otherwise symmetrical with no
scars seen.
Palpation
The apex beat was
palpable on the 5th intercostal space at the midclavicular line.
There were no
heaves and thrills.
Auscultation
Both heart sounds are
heard in all areas with splitting of the heart sounds nor any additional heart
sounds.
Abdominal Examination
Inspection
The abdomen is
scaphoid in shape with no visible scars seen.
The umbilicus is
centrally located and inverted.
There was no
dilated veins.
Palpation
There were no
tenderness, rebound tenderness or guarding seen.
There is no
palpable mass and the liver and spleen is not palpable.
Auscultation
Bowel sounds are
heard every 2 seconds and is gurgling in nature.
There are no renal
or aortic bruits heard.
Provisional Diagnosis
Pulmonary
Tuberculosis
Differential Diagnosis
Pneumonia
Acute Exacerbation
of Chronic Obstructive Airway Disease (AECOAD)
Pulmonary Embolism
Investigation
1) Full Blood Count
|
Test
|
Value
|
Units
|
|
WBC
|
6.6
|
X
103/ µL
|
|
RBC
|
4.15
|
X
103 / µL
|
|
HGB
|
12.0
|
g/Dl
|
|
HCT
|
36.8
|
%
|
|
MCV
|
88.7
|
fL
|
|
MCH
|
28.9
|
pg
|
|
MCHC
|
32.6
|
g/dL
|
|
PLT
|
340
|
X
103 / µL
|
|
LYM%
|
18.7
|
%
|
|
MXD%
|
16.5
|
%
|
|
NEUT%
|
64.8
|
%
|
|
LYM#
|
1.2
|
X
103 / µL
|
|
MXD#
|
11.1
|
X
103 / µL
|
|
NEUT#
|
4.3
|
X
103 / µL
|
|
RDW
|
46
|
fL
|
|
PDW
|
8.6
|
fL
|
|
MPV
|
7.6
|
fL
|
|
P-LCR
|
9.1
|
%
|
2) Blood Urea & Serum Electrolyte (BUSE)
|
Code
|
Test Name
|
Results
|
Reference
Interval
|
Units
|
Comments
|
|
BUN
|
Blood
Urea Nitrogen
|
2.8
|
2.5
– 6.4
|
mmol/L
|
Normal
|
|
Na
|
Sodium
|
139
|
136
– 145
|
mmol/L
|
Normal
|
|
K
|
Potassium
|
3.6
|
3.5
– 5.1
|
mmol/L
|
Normal
|
|
Cl
|
Chloride
|
105
|
98
– 107
|
mmol/L
|
Normal
|
|
TP
|
Total
Protein
|
73.7
|
64.0
– 82.0
|
g/L
|
Normal
|
|
GLOB
|
Globulin
|
50.1
|
30.0
– 62.0
|
g/L
|
Normal
|
|
ALB
|
Albumin
|
23.6
|
34.0
– 50.0
|
g/L
|
Low
|
|
TB
|
Total
bilirubin
|
11.3
|
3.0
– 17.0
|
µmol/L
|
Normal
|
|
ALT
|
Alanine
Transaminase
|
26
|
12
– 78
|
U/L
|
Normal
|
|
ALP
|
Alkaline
Phosphatase
|
68
|
46
- 116
|
U/L
|
Normal
|
3) Mantoux test
Result : 7mm
(normal)
4) Sputum Collection
Gram stain
* no leucocyte
seen
* moderate
epithelial cells seen
* numerous gram
positive cocci seen
* moderate gram
positive bacilli seen
* scanty gram
negative bacilli seen
* scanty yeasts
seen
Culture
* no significant
growth (Culture & Sensitivity)
5) HIV Serology
HIV 1 & 2
Combo Ab+Ag (CMIA) : Non-reactive
6) Hepatitis Serology
*Hbs Antigen detected
*Anti HCV Screen
(CMIA) : Reactive
*HCV Ab detected
in this blood sample
7) Lactate Dehydrogenase
Result : 378 U/L
(Normal : 240-480)
8) Pleural Biopsy & Tapping
*multiple
adhesions seen
*adhesions with
unhealthy looking parietal pleura
*white patches
thick layer covering the parietal pleura
*no sago nodules
seen
|
Test
|
Result
|
Unit
|
|
Fluid Type
|
Pleural
|
-
|
|
Fluid pH
|
7
|
-
|
|
Fluid Glucose
|
4.0
|
mmol/L
|
|
Fluid LDH
|
354
|
U/L
|
|
Fluid Total
Protein
|
49.2
|
g/L
|
9) ECG


10) Chest X-ray
Management
Continue anti-TB
drugs (Akurit-4)
Off Tramal
Trace pleural
biopsy, MTB C&S and Pathogen
Keep ICT
Refer for chest
physio
Discussion
This patient is 52
years old gentleman living at Setapak, Kuala Lumpur who presented with a chief
complaint of fever and chest pain for the past one month. From the history, the
patient lived at overcrowded place, had close TB contact, illicit drug user,
chronic smoker and alcoholic which are the important high risk factor according
to CPG.
Patient presented
with chest pain and fever for 6 months, however, adult patients with active PTB
typically presents with a history of chest symptoms such as productive cough,
hemoptysis and chest pain and also nonspecific constitutional symptoms such as
loss of appetite, unexplained weight loss, fever, night sweats and fatigue.
This patient does not have hemoptysis, productive cough, dyspnea and night
sweats.
The diagnosis of
TB is supported by imaging and laboratory tests. However, diagnosis is
confirmed by isolating Mycobacterium tuberculosis from clinical samples. In
this patient, FBC, BUSE, Mantoux test, sputum culture, HIV serology, hepatitis
serology, lactate dehydrogenase, pleural biopsy and tapping, ECG and chest
X-ray. Out of that, the positive findings were low albumin in BUSE, presence of
moderate gram positive bacilli seen in sputum gram stain, presence of HCV Ab in
hepatitis serology test, multiple adhesions seen in pleural biopsy and tapping
and left sided lower and middle zone opacity in chest X-ray.
This patient was
continued with anti-TB drugs which is Akurit-4. Akurit-4 are combination of
ethambutol, isoniazid, rifampicin and pyrazinamide. 4 drug combination :
Isoniazid 75 mg, Rifampicin 150 mg, Pyrazinamide 400 mg and Ethambutol 275 mg
tablet.
References
1. CPG- Management
of Tuberculosis (3rd Edition)
Subscribe to:
Comments (Atom)